


Meet Nayya: The agentic AI adviser optimizing health and wealth for all


Our mission: To create a future where AI turns overwhelming benefits choices into clear paths, where intelligence anticipates needs, and guidance arrives ahead of the question.
This is the future we are building.
Join our movement.
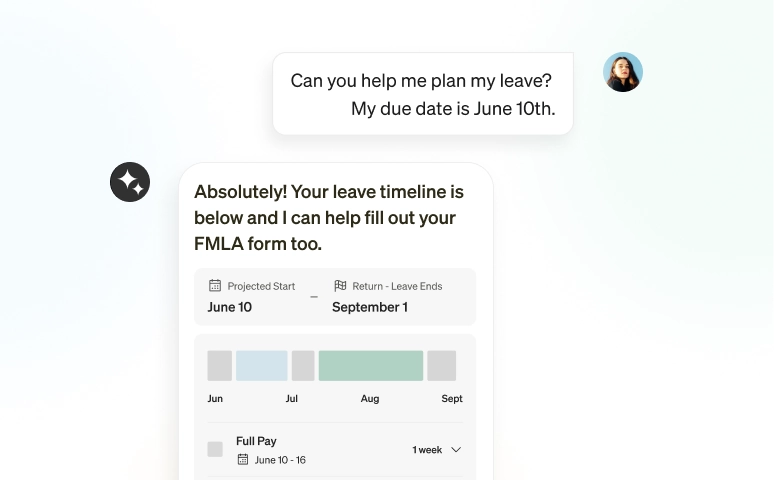
While others provide guidance, Nayya provides results. Employees choose how much we do, from answering benefits questions to taking actions on their behalf.
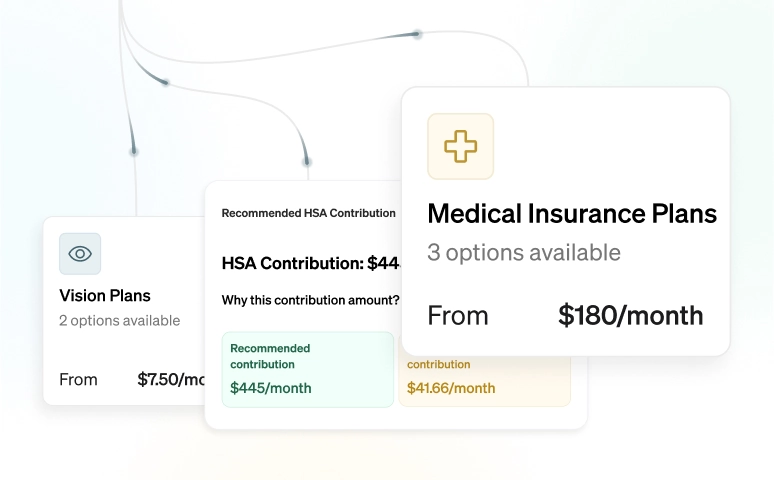
Health impacts wealth. Wealth enables health. Nayya uses machine learning to optimize both together, maximizing value across every benefit dollar.
Nayya integrates seamlessly into Slack, Teams, iMessage, and everywhere people work. No more abandoned portals. Just intelligence where you need it.
An AI platform that gets smarter, faster, and more personal over time.


We uphold the highest standards in data privacy, security, and accessibility by adhering to the following compliance measures: HIPAA, WCAG AA 2.1, SOC 2 + HITRUST, ADA, CCPA, and NIST 800.

